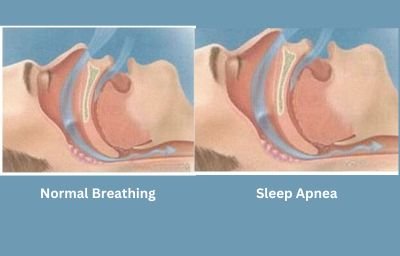
Snoring occurs when air moving through the nose and throat during sleep passes through a narrowed area which cause the structures to vibrate and rattle causing the familiar sound of snoring.
Obstructive Sleep Apnea (OSA) is a common disorder in the Canton area involving collapse of the upper airway during sleep. This repetitive collapse results in frequent awakenings and tiredness during the day, even with adequate sleep time. As specialists in upper airway anatomy, physiology and surgery, We are uniquely qualified to treat patients with OSA. In the Clinical Guidelines for Evaluation, Management and Long-term Care of Obstructive Sleep Apnea in Adults, it is recommended that evaluation for primary surgical treatment be considered in select patients who have severe obstructing anatomy that is surgically correctible (e.g., large tonsils blocking the throat) and in patients in whom continuous positive airway pressure (CPAP) therapy is inadequate.(Epstein, EJ, Evidence Based Clinical Guideline)
Surgical treatment of pediatric sleep disordered breathing with tonsillectomy and adenoidectomy is the recommended first line treatment. In the pediatric population, resolution of OSA occurs in 82% of patients who are treated with tonsillectomy and adenoidectomy.
In most patients with moderate to severe sleep apnea, continuous positive airway pressure (CPAP) is the first line treatment. Successful long term treatment of OSA with CPAP is difficult to achieve and fewer than 50% of patients on CPAP are adequately treated, as defined by 4 hours of use 70% of nights. Other treatment options must be available to patients with OSA.
Surgical procedures may be considered as a secondary treatment for Obstructive Sleep Apnea when the outcome of CPAP therapy is inadequate, such as when the patient is intolerant of CPAP, or CPAP therapy is unable to eliminate OSA. Surgery may also be considered as a secondary therapy when there is an inadequate treatment outcome with an oral appliance (OA), when the patient is intolerant of the OA, or the OA therapy provides unacceptable improvement of clinical outcomes of OSA (Consensus). Surgery may also be considered as an adjunct therapy when obstructive anatomy or functional deficiencies compromise other therapies or to improve tolerance of other OSA treatments Surgery for OSAS has been shown to improve important clinical outcomes including survival and quality of life
When CPAP is inadequate to control the symptoms of sleep apnea, and after examination, there is found to be a site of obstruction with the tonsils, adenoids, or nasal septum, surgery may be recommended. Surgery is designed to remove the tonsils and a small portion of the uvula and soft palate. This has the net effect of opening the inlet of breathing at night, reducing or eliminating the need for CPAP. Afterwards, weight loss and regular aerobic activity is encouraged to maintain results.
After a thorough history and physical examination an overnight sleep study may be recommended to determine if sleep apnea is present. A new device, which allows home sleep study, is available. This is more convenient and less expensive for most patients. Please watch the video on the home sleep study device.